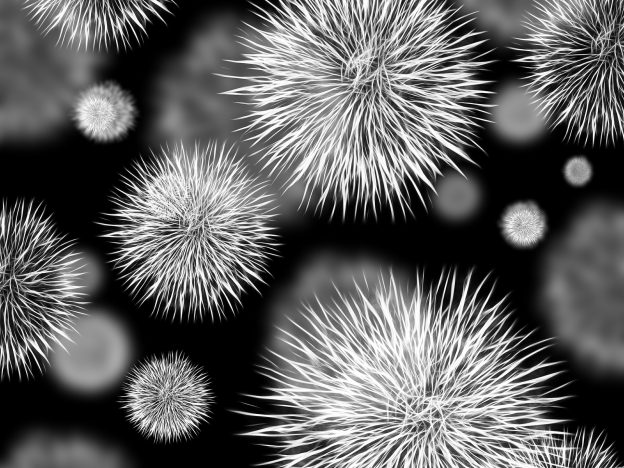
The Borrelia bacterium, which exists in ticks, can develop into an infectious disease in humans when bitten. This disease is known as lyme disease (or Lyme Borreliosis) Infections have previously been associated with an increased risk of suicidal behavior. Trine Madsen from DRISP has, in collaboration with colleagues, investigated whether Lyme Borreliosis was linked to increased prevalence of psychiatric diseases and suicidal behavior.
Using register data for all persons living in Denmark from 1994 to 2016 (n=6,945,837), patients diagnosed with Lyme Borreliosis were identified based on hospital diagnoses. Their risk of developing psychiatric diseases and suicidal behavior was analyzed.
The results showed that persons who developed Lyme Borreliosis (i.e., an infection after a tick bite) had a 1.3-fold higher rate of psychiatric diseases, as well as a 2-fold higher rate of suicide attempts and a 1.75-fold higher suicide rate when compared to the background population. The highest risk of developing a psychiatric disease was observed within the first 6 months after persons developed Lyme Borreliosis. If the person had had multiple incidents of Lyme Borreliosis, this was associated with an increasing risk of suicide attempts.
In conclusion, the study showed that persons diagnosed with Lyme Borreliosis at Danish hospitals have an increased prevalence of psychiatric diseases, suicide attempts and suicide.
You can find the study here: https://ajp.psychiatryonline.org/doi/10.1176/appi.ajp.2021.20091347
DRISP: Trine Madsen, Merete Nordentoft & Annette Erlangsen
Partners:
- Michael Eriksen Benros, Research Unit, Mental Health Centre Copenhagen
- Brian A. Fallon, MD, Center for Neuroinflammatory Disorders and Biobehavioral Medicine and director of the Lyme and Tick-Borne Diseases Research Center at Columbia University, USA